LifeNabled – On a mission to provide prosthetics for recipients living in a remote area of Guatemala, LifeNabled’s volunteers digitised their design and manufacturing workflow, enabling them to rapidly increase the number of patients they could help and improve prosthetic devices at the same time
LifeNabled is a charity established in 2006 to provide free clinics and prosthetics to those in need in remote areas of the northern Petén region of Guatemala.
It’s a region where poverty is widespread. Many people there survive and feed their families on just $3 dollars a day. Surrounded by dense jungle, the inaccessible nature of many villages means there’s zero access to basic medical care, let alone prosthetic services.
Losing mobility in an area like this often means missing out on education or being unable to provide for your family. Stigma around disability adds to the desperate situation many find themselves in.
LifeNabled’s volunteers first began to tackle this challenge with traditional fabrication methods. That involved taking a cast of an amputee’s remaining limb during an evaluation session, and then using the cast to create a custom mould to thermoform the socket. The socket would then be connected to off-the-shelf components in order to manufacture the necessary prosthesis. Finally, the prosthetist would fit the device to the patient and make necessary adjustments to ensure a good fit.
But evaluating, manufacturing and fitting prosthesis to the 30 to 50 patients they would see at its week-long clinics took a real toll on the LifeNabled volunteers. That prompted the charity, cofounded by prosthetist/orthotist Brent Wright and his wife Meredith Wright, to reassess its processes. As part of that overhaul, it has recently taken steps to fully digitise the design and manufacturing stages that require the most expertise.
The far more efficient new process worked like this: First, two team members flew to Guatemala to take 3D scans of patients. In just two days, they were able to evaluate 35 amputees.
Then, using the scan data, Brent Wright was able to design and customise each device and manufacture the sockets using HP’s MultiJet Fusion 3D printing technology from his base in North Carolina.
Finally, the team returned to Guatemala a month later to deliver the devices and fit them to patients, who left the clinics walking on some of the most advanced prostheses in the world.
Inner lining technology
Essential to the new prosthesis design was its inner liner. This is designed to ensure that the socket remains comfortable for the wearer, even after hours of use. Moreover, it must be breathable for hygiene reasons – a particularly important point in the hot, humid jungle environment of this region of Guatemala.
But traditional gel-like inner liners restrict airflow, cost more than $160 each, and have a limited lifespan of only three to six months in this kind of environment. In other words, these represented a prohibitive expense for the target audience in this case.

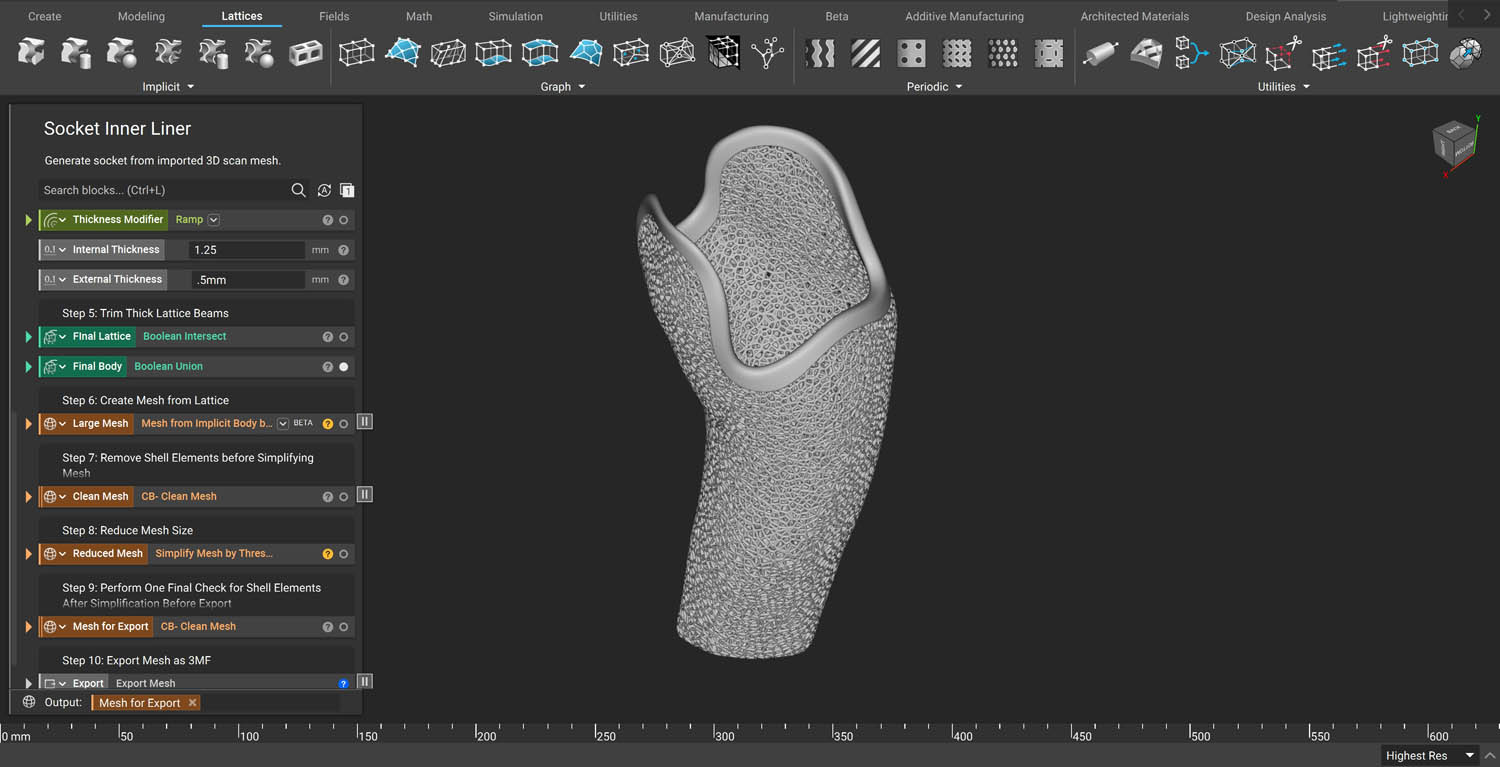
Instead, 3D-printed foam provided the answer. Flexible inner socket liners feature lattice structures capable of imitating the properties of traditional foams. These are manufactured from an elastic TPU material and offer the design additional benefits.
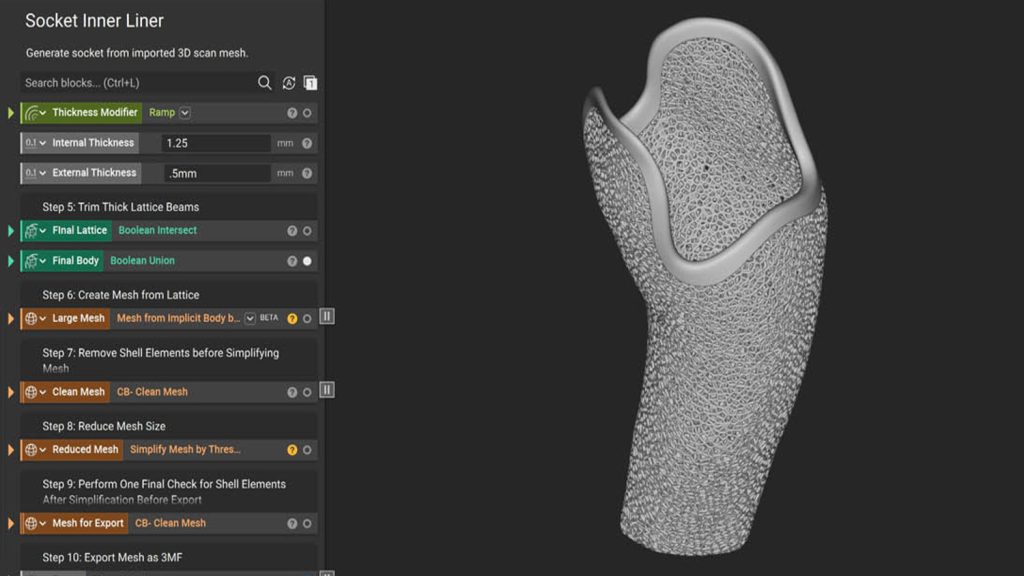
For example, properties can be tuned from soft foam to stiff plastic according to the physiology or preferences of the patient. This effect was achieved by closely controlling the design input parameters of the lattice, such as beam thickness and porosity, using nTopology.
Without nTopology, Wright says this step would have been a “brutal process”, since the software he previously used for such work would often take hours to generate a result.
“Designing custom flexible inner liners was going to be a challenging task if we would do it in any other software other than nTopology. Once the workflow was done, all I had to do was to swap out meshes. The process ran over and over again,” he says.
Using the mesh of the patient’s 3D scan data as input, a shell with variable thicknesses was generated. nTopology’s latticing blocks were then used to create a flexible inner liner that provided the necessary level of cushioning. To repeat the process and generate a new design, LifeNabled’s designers only had to swap in a new input mesh with 3D scan data from another patient.
With nTopology’s reusable workflows, the team says it saved more than a whole day of error-prone computational processing during the design phase and produced higher quality and error-free results.
To manufacture the parts, the team opted for HP’s Multi Jet Fusion 3D printing process and its TPU material, which contributed overall to the digital process that saved the team on average three days of fabrication and replaced a laborious manual step with streamlined digital manufacturing.
This is a human story. This is not a story of how we get a profit out of humans. It’s a story about how we get people walking
LifeNabled – next steps
Wright says that with 3D printing systems located worldwide, even in developing countries, the next step is to scale the digital process and create a global network.
Local physicians can be trained through video calls to evaluate patients and fit prostheses. As for the design of devices, this can be generated using the automated processes that the team has developed.
“There are millions of people that need prostheses worldwide,” says Wright. “It’s a team effort to reach all of them. This is a human story. This is not a story of how we get a profit out of humans. It is a story of how we get people walking.”
From a technical perspective, Wright continues to refine his designs to make them even more cost-effective. For example, his team is currently creating lighter socket ribs with a simulationdriven geometry using a field-driven design approach.
People who could not possibly afford a prosthesis now have access to some of the best in the world, helping them take steps towards a better life.